
The air expands the colon, which provides a better view of the colon lining. The sigmoidoscope contains a light and a tube that allows the doctor to place air into your colon. The doctor will insert a sigmoidoscope into your rectum. Wearing a gown, you'll begin the exam lying on your left side on the exam table, usually with your knees drawn toward your abdomen. You may need to adjust your dosages or stop taking the medication temporarily. Remind your doctor of your medications at least a week before the exam - especially if you have diabetes, if you take medications or supplements that contain iron, or if you take aspirin or other blood thinners. You will need to use an over-the-counter enema kit - typically a few hours before the exam - to empty your colon.

If your doctor asks you to take a laxative, it will be in either pill or liquid form.
Take a laxative the night before the exam. You may be asked not to eat or drink anything after midnight the night before the exam. Drinks may be limited to clear liquids - plain water, broth, carbonated beverages, and tea and coffee without milk or cream. Your doctor may ask you not to eat the day before the exam. Follow a special diet the day before the exam. To empty your colon, follow your doctor's instructions carefully. Any residue in your colon may obscure the view of your colon and rectum during the exam. Bleeding from the site where a tissue sample was takenīefore a flexible sigmoidoscopy exam, you'll need to empty your colon. Rarely, complications of a flexible sigmoidoscopy exam may include: Request an Appointment at Mayo Clinic RisksĪ flexible sigmoidoscopy exam poses few risks. There is a lower risk of direct harm such as a tear in the colon or rectum wall (perforation) with sigmoidoscopy, compared with colonoscopy. In addition, an anesthetic is often not required. Sigmoidoscopy may occasionally be preferred over colonoscopy because the preparation for sigmoidoscopy and the test itself may take less time. Talk with your doctor about your options. Sigmoidoscopy is one option for colon cancer screening, but there are other options that allow your doctor to view your whole colon, such as colonoscopy. If you're age 50 or older and you have no colon cancer risk factors other than age - which puts you at average risk - your doctor may recommend a flexible sigmoidoscopy exam every five years to screen for colon cancer. 
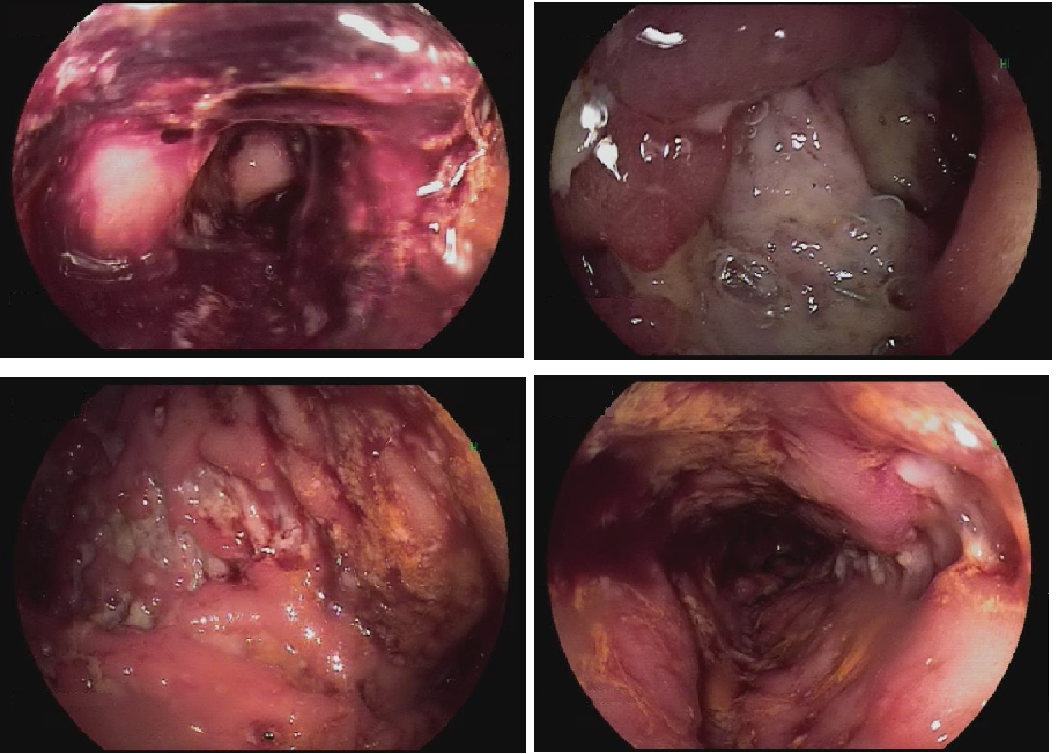
A flexible sigmoidoscopy exam can help your doctor explore possible causes of abdominal pain, rectal bleeding, changes in bowel habits, chronic diarrhea and other intestinal problems.
Investigate intestinal signs and symptoms. There is a learning curve involved in such procedure and it can easily be overcome in high volume centers.Ĭolorectalanastomosis minimally-invasivesurgery oncologicalandfunctionaloutcomes restorativecolorectalresection splenicflexuremobilization.Your doctor may recommend a flexible sigmoidoscopy exam to: Conclusions: In our perspective, the routine mobilization of the splenic flexure as a first step of the colorectal restorative resections associate many advantages and these strategies should be largely used. The mean follow-up for these patients is 7 months (range, 4-12 months). No early cancer recurrence, deaths or major complication were encountered. No intraoperative incidents were associated with the SFM. The robotic approach has been used in 40% (16 patients). There were 30 patients with rectal cancer, 10 with sigmoidal tumors, five with sigmoidal resection for diverticulitis and Hartmann reversal was indicated in two. Results: Between January and December 2018, 47 patients had SPM as a first step of the performed colorectal procedure in our institution. However, the combination of different maneuvers for an easier, safer approach decreases the morbidity and is saving surgical time. 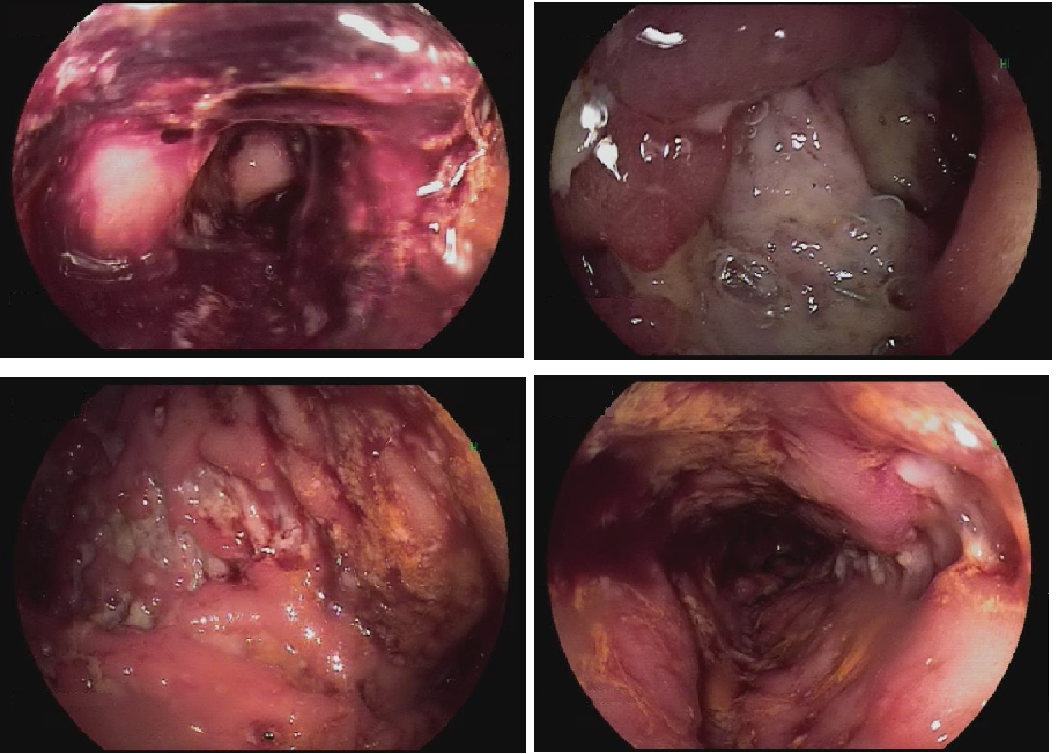
There are four routes for SFM: two from medial to lateral, one starting from the splenic vein the other one from the promontory, a superior to inferior approach and a lateral to medial approach. Method: A detailed description of the laparoscopic surgical technique for SFM is performed. The aim of this paper is to describe the technique of laparoscopic splenic flexure mobilization and to discuss the advantages of using it as the first surgical step in colorectal rectal resection analyzing our last 12 months experience (2018). Looking for improved expertise and better outcomes, in 2016, we have decided to routinely perform SFM as a first step of all the laparoscopic or robotic sigmoid and rectal resections. However, the surgical procedures are technically complex thereby overcoming the learning curve may not be an easy process.

Background: Mobilization of the colonic splenic flexure (SFM) is an essential surgical step of the restorative rectal resections.







 0 kommentar(er)
0 kommentar(er)
